

Our doctors will discuss the benefits, risks and complications of any glaucoma treatments with you during your appointment.
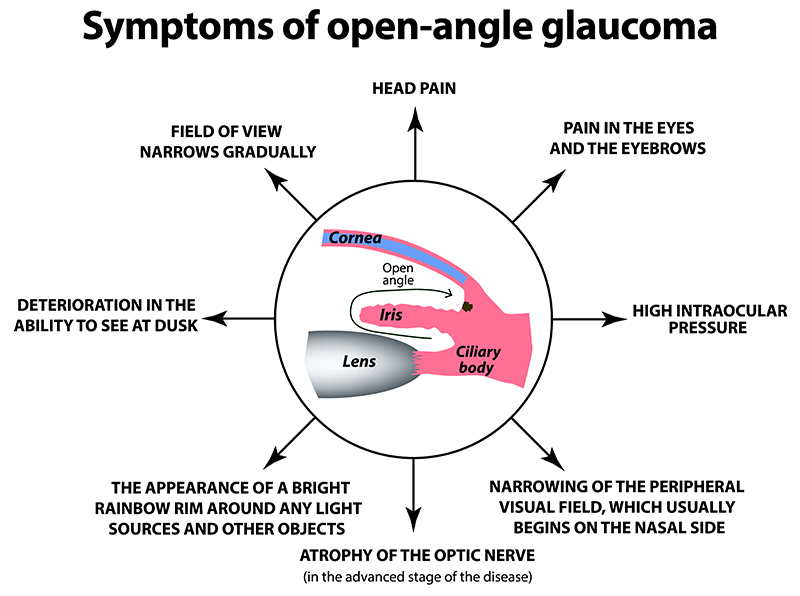
Initial options in the treatment of glaucoma typically include pressure lowering drops and/or laser treatment. Drops commonly work by decreasing the amount of fluid produced by the eye, which usually results in lower pressures. Medications can also increase the amount of fluid that leaves the eye. While drops cannot cure the disease, in most cases, the use of these medicated eye drops can slow or halt the worsening of glaucoma. There are 256 combinations of drops that can be used and as a result surgery is not frequently needed.
If drops do not provide sufficient treatment, laser therapy in the form of an argon laser trabeculoplasty or selective laser trabeculoplasty, may be recommended. Our doctors will speak with you and help you understand your glaucoma and which options will be best for your situation. At EPLB, we can perform both Argon and Selective laser trabeculoplasty. The both involve increasing the flow of fluid out of the eye. The benefits of SLT include the fact that it can be repeated and causes less damage to the drainage system of the eye.
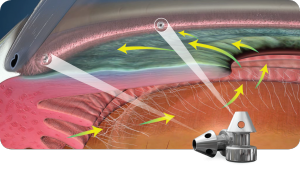
Have glaucoma but also preparing to have your cataracts removed during cataract surgery? The iStent inject may be right for you!
The iStent inject has helped millions with glaucoma manage their intraocular pressure levels. Why not take advantage of this once in a lifetime opportunity?
During cataract surgery, you can address your cataracts and glaucoma at the same time.

When you get the iStent inject, it includes two small implants. These small implants make up the world’s smallest medical device implanted in the human body.
Worldwide, Glaukos devices have been implanted in hundreds of thousands of eyes. Every day, more and more patients benefit from the convenience of this technology.
For glaucoma patients who receive the iStent inject, it’s life-changing! After the iStent implant has been implanted, the device restores normal intraocular pressure. The iStent inject was created to:
Depending on the patient, you may be able to reduce or cut out taking glaucoma medication.
The Glaukos iStent inject is comprised of two tiny implants. Each of these tiny implants is made of surgical titanium. After implantation of the iStent inject, you won’t see or feel the stents.
To control the increased intraocular pressure, the iStent inject creates two openings. These openings are between the front part of your eye and its natural drainage pathway.
These openings exist to help increase the flow of fluid in your eye. By creating permanent bypasses through the trabecular meshwork, the Glaukos iStent inject:
Only patients with glaucoma and cataracts can get the iStent inject. This is a procedure that is only performed in conjunction with cataract surgery.
You cannot have the iStent inject if you don’t have cataracts or don’t need cataract surgery. In most cases, the iStent inject should not be your first treatment for glaucoma.
You shouldn’t undergo implantation of the iStent inject if you’ve had a glaucoma procedure in the last 90 days. Go over your medical history with your doctor before undergoing any procedure.
Use your appointment to ask any questions or go over any concerns that you may have. This is the best time to find out if the iStent inject could be a procedure for you to consider!
Wondering if the iStent inject could be right for your glaucoma and cataract needs? Schedule an appointment at Eye Physicians of Long Beach in Long Beach, CA today!
For qualified patients, the iStent inject is a safe way to remove cataracts and lower intraocular pressure!
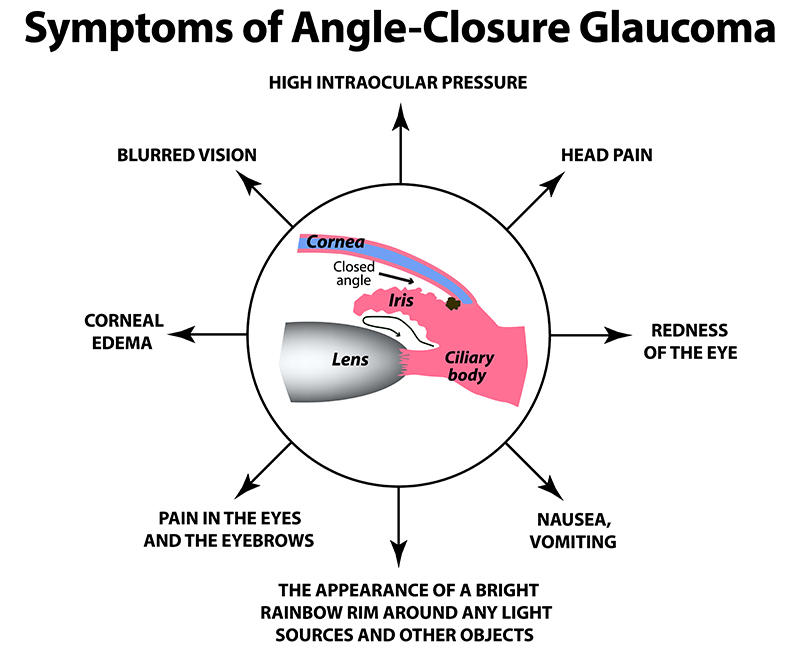
In the case of angle closure, the physician will need to remove the blockage to reduce the pressure. In this case, a peripheral iridotomy or a peripheral iridoplasty are more appropriate. In both cases, the purpose of the laser is to pull the iris away from the angle. In a peripheral iridotomy, the surgeon will create a small opening in the peripheral iris and stabilize the pressure behind and in front of the iris, pushing the iris back. This works when the mechanism of angle closure is that the pupil gets too close to the lens, preventing the fluid from behind the iris to come around, causing a buildup behind the iris. The laser creates a new path for fluid and releases the increased pressure. In a peripheral iridoplasty, the laser is used to shrink the mid peripheral iris, pulling it away from the drainage system.
The next level of therapy if laser and eyedrops fail, consists of incisional surgery, or surgery that involves cutting. Our doctors may recommend one of a variety of surgical procedures for the treatment of your glaucoma, and a trabeculectomy is one of the available options. A small incision will be made into the drainage system of the eye and a new channel for the fluid created, which then flows under or oozes through the conjunctiva. This allows for increased ouflow of fluid and a reduction in pressure. A small bubble will appear on the conjunctiva at the point of intersection of the cornea and the sclera. Other surgical procedures include trabectome, goniotomy, canaloplasty, and endoscopic cyclophotocoagulation.
Other options include shunts are small artificial devices that are surgically attached to the eye’s surface for treatment of glaucoma. The devices have a tiny tube that is inserted in the eye and creates a passageway for the fluid to escape. The shunts and implants allow fluid to escape the eye without having to pass through the damaged trabecular meshwork. Shunts are made of materials such as polypropylene and silicone and depending on the type of glaucoma, the shunts may either be hollow to improve drainage or have valves to control the drainage. The main shunts used are Baerveldt shunts (no valve) or an Ahmed shunts which have a valve. A newer shunt is the Express Shunt. This procedures combines the benefits of a shunt with that of a trabeculectomy.