

Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness in American adults. The retina is the like the film in a camera; in which it is the light sensing film on the back of the eye that captures the images. In Diabetes, sugar (glucose) builds up within blood vessels in the retina and tissues of the body causing glucose to attach to the proteins in the wall. This alters their normal structure and functioning. The vessels eventually get blocked, break, and leak, or swell and leak fluid. When they cannot deliver an adequate amount of blood supply to the eye, the eye can generate abnormal new blood vessels.
Early diabetic retinopathy usually has no symptoms. However, worsening diabetic retinopathy can lead to visual loss and blindness.
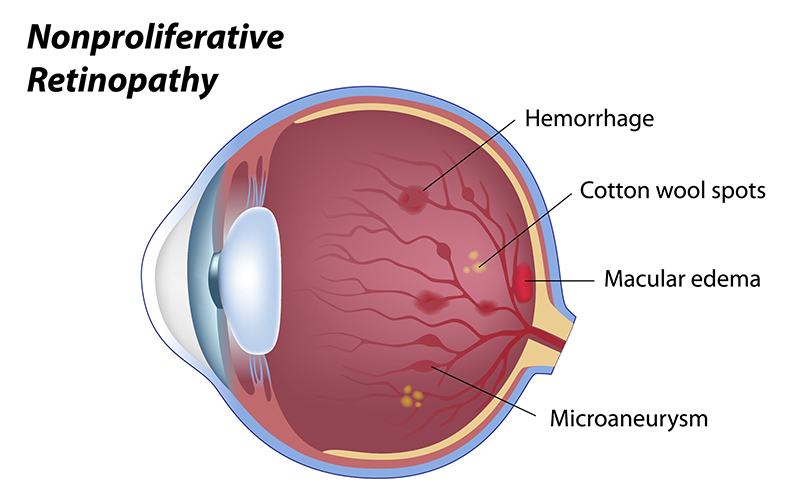
Nonproliferative Retinopathy – in the earliest stages of diabetic retinopathy, small areas of balloon-like dilatation of the retinal blood vessels occur called microaneurysms. Initially, these blood vessels leak blood, water, or cholesterol. The result is swelling, bleeding, or lipid deposition within the retina or any combination of the three. When leakage causes swelling within the central portion of the retina, macular edema occurs and the blood vessels can later become blocked. When enough of the blood vessels become blocked, the retina becomes deprived of blood supply and signals to the body to build new blood vessels. When these new vessels start to grow, this marks the beginning of the next stage of diabetic retinopathy, proliferative diabetic retinopathy.
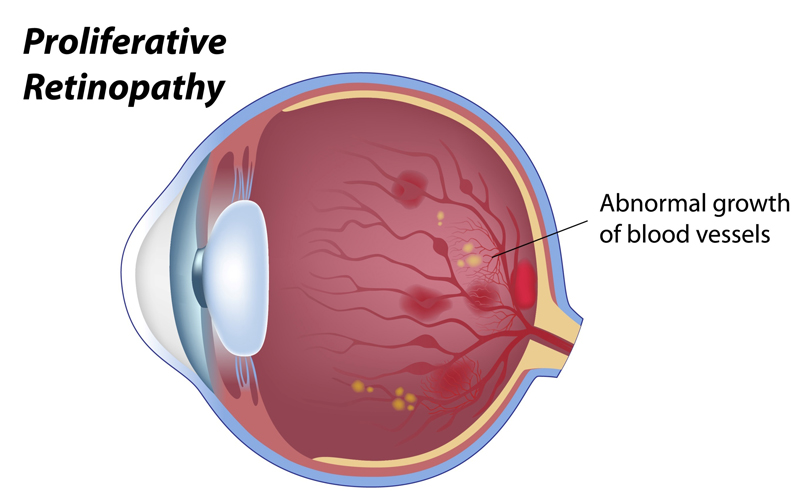
Proliferative Retinopathy – At this stage, new vessels are growing to feed what is otherwise an eye missing blood. These vessels can grow on the retina, optic nerve, iris or into the vitreous gel inside the eye, and tend to grow poorly and are very fragile. If these fragile vessels break, they can lead to large hemorrhages on the surface of the retina or within the vitreous. These vessels can also cause scar tissue leading to distortion and eventually pull the retina away from the rest of the eye, a tractional retinal detachment. The blood vessels growing within the iris can lead to glaucoma by occluding the internal drainage of the fluid that nourishes the front of the eye.
Blood sugar control is paramount. Genetic factors are also important, as variations in several genes have been found to be associated with an increased risk for developing diabetic retinopathy. These genes have been demonstrated through genetic linkage as well as genetic associations. The rates of progression are different for those with northern European descent than for African- and Hispanic-Americans who have higher rates of retinopathy progression. However, although some of the progression of retinopathy may be controlled by genetic factors, as there is no question diabetic retinopathy is a complex disease with many affecting factors. The duration of diabetes is probably the strongest predictor for the development and progression of retinopathy. Among younger-onset patients with diabetes in the Wisconsin Epidemiologic Study of Diabetic Retinopathy, the prevalence of any retinopathy was 8% at three years, 25% at five years, 60% at ten years, and 80% at fifteen years.
Studies have definitively demonstrated that better blood sugar control slows the onset and worsening of retinopathy. The rates of progression correlate with HbA1c levels (Glycosylated hemoglobin). The HbA1c is a blood test that gives you a picture of what your blood sugars have been doing during the two to three months prior to the test. Studies also show controlling your blood pressure and cholesterol will also help minimize the damage. Exercise, both muscle building and aerobic, and maintaining good overall health have been shown to decrease the need for insulin and decrease the risk of diabetic complications.

Initially, nonproliferative diabetic retinopathy may have no symptoms. Retinal swelling due to leakage of fluid from retinal blood vessels will cause blurred vision and/or distortion. Displacement of the receptors within the retina can cause objects to look smaller, larger, blurred or distorted.
Bleeding will mechanically block the incoming image. This may lead to the appearance of floaters or the impression that there is something blocking your vision. If you suddenly see spots in your vision, see your ophthalmologist as soon as possible. You may need treatment before more serious bleeding occurs. Occasionally, the bleeding can stop and the spots can disappear, but bleeding can reoccur and cause severely blurred vision. In addition, if left untreated, proliferative diabetic retinopathy will be more likely to cause severe vision loss and even blindness. The earlier you receive treatment, the more likely the treatment will be effective.
Cholesterol deposits will have combined effects of fluid and bleeding. All of these will also interfere with metabolism and the health of the light receptors within the retina.

Diabetic retinopathy is detected through eye exams. Diabetic eye exams as recommended by your primary care doctor and your ophthalmologist are very important. In the early stages, a yearly exam may be adequate, but more exams may be needed as often as every few months for monitoring patients with advanced diabetic retinopathy. Your ophthalmologist will monitor your eye for evidence of leaking blood vessels and associated signs if diabetes. Your doctor may do this by performing dilated eye exams. Clinical examination is superior for detecting retinal thickening from macular edema and the early detection of new vessels than photography. Retinal photography also requires both a trained photographer and a trained reader. As a result, photography is not usually used in isolation as a screening method for diabetic retinopathy.
In order to better understand the circulation within the retina, your doctor may do fluorescein angiography. During this test, a special vegetable dye is injected in your arm and photographs are taken as the dye travels through the blood vessels in the retina. This test accurately pinpoints which vessels are leaking and the extent of blockage. This test is also used to guide the treatment of macular edema. Eye Physicians of Long Beach has the ability to do all of these tests, including digital photography and intravenous fluorescein angiography.
In many cases, our doctors can do a simple test called optical coherence tomography (OCT) to determine qualitative and quantitative estimates of retinal thickness. This machine uses patterns of interference of light to take pictures of the cells within your retina with resolution of less than 10 microns. Using this, the doctors at Eye Physicians of Long Beach may be able to detect macular edema before it damages your vision.
People with diabetes should control their levels of blood sugar, blood pressure, and blood cholesterol. Exercise can also improve the amount of blood supply to the eye. Treatment can include laser, intravitreal injections, and vitrectomy, as discussed below.
Macular edema (swelling of the central portion of the retina) can be treated with laser applied to focal areas of leakage. Laser spots can close areas of leakage. The Early Treatment Diabetic Retinopathy Study demonstrated the effectiveness of focal photocoagulation in eyes with macular edema and in cases where the areas of leakage are too close to the macula, injections of steroids in the eye may help.

Proliferative retinopathy results in bleeding inside the eye and is usually treated with laser therapy. During panretinal photocoagulation (PRP), your doctor will place between 1,200 to 2,000 laser burns in the areas of the retina suffering from low blood supply; this usually causes the blood vessels to retreat. This type of laser can cause problems with night vision and decrease peripheral vision, but without it, there is a very high risk of blindness. The best approach to diabetes is to avoid retinopathy, but if the proliferative disease is diagnosed, the laser can save the vision. The Diabetic Retinopathy Study (DRS) investigated if scatter (panretinal) photocoagulation could reduce the risk of vision loss from proliferative retinopathy. After only 2 years, photocoagulation was shown to significantly reduce severe visual loss.
If the bleeding is severe, you may need a surgical procedure called a vitrectomy. During a vitrectomy, blood is removed from the center of your eye.
The laser does not cure diabetic retinopathy. Since diabetes is a problem that affects your whole body, it affects all of the vessels of the retina, as well as other areas. The best way to handle diabetic retinopathy is through prevention with blood sugar control and exercise.